What’s Wrong With the Baby Friendly Hospital Initiative? I’m Glad You Asked.

For those who are no longer entrenched in the newborn and infant stages, the Baby Friendly Hospital Initiative “BFHI” was a global initiative launched by the World Health Organization and United Nations Children’s Fund in the early 1990’s to “encourage and recognize hospitals and birthing centers that offer an optimal level of care for infant feeding and mother-baby bonding. It recognizes and awards birthing facilities who successfully implement the Ten Steps to Successful Breastfeeding (i) and the International Code of Marketing of Breast-milk Substitutes (ii).” Essentially, it is a program that is supposed to encourage and promote breastfeeding as well as skin-to-skin bonding. Unfortunately, what started off as a good intention (we all know what the road to hell is paved with), has become a euphemism for a campaign that has sacrificed and marginalized maternal physical and mental health, and the health of newborns, for the sake of its’ bottom line.
The bottom line of the BFHI is to make as many mothers breastfeed as possible. In order to do this, the BFHI requires designated facilities to follow it’s ten-step recommendation:
Have a written breastfeeding policy that is routinely communicated to all health care staff.
Train all health care staff in the skills necessary to implement this policy.
Inform all pregnant women about the benefits and management of breastfeeding.
Help mothers initiate breastfeeding within one hour of birth.
Show mothers how to breastfeed and how to maintain lactation, even if they are separated from their infants.
Give infants no food or drink other than breast-milk, unless medically indicated.
Practice rooming in – allow mothers and infants to remain together 24 hours a day.
Encourage breastfeeding on demand.
Give no pacifiers or artificial nipples to breastfeeding infants.
Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or birth center.
Let me preface this by stating that I am not anti-breastfeeding. If you want to do it, great. My problem with the BFHI is that it has taken the goal of breastfeeding to an extreme, making it the priority above all else, including the health of the baby and the mother. Because of this, the BFHI is not really “mother-friendly” at all, and even not as “baby friendly” as it claims.
My biggest issues with the BFHI are as follows. First, it does not support feeding choice, despite what may be right for the baby or for the mother. It is one thing to tell the mother about the benefits of breastfeeding and to have lactation support in the hospital. It is completely another to hide formula and to force new mothers who bottle feed to sign waivers. We trust mothers to make their own choices about sleeping arrangements, clothing, diapering, and education. It is ridiculously patronizing to refuse to let them make their own choices about feeding.
Second, many hospitals, in a frenzied rush to receive the BFHI designation, have done away with their well-baby nurseries. The ostensible reason for this move is because “babies and mothers sleep better when they room in”. I don’t care what any study allegedly says, go ahead and re-read that last line again with a straight face. (When they told this to my husband and I for our third child’s birth we laughed so hard we almost fell out of our chairs at the hospital orientation). Of course, hospitals are more than happy to jump on the no-nursery bandwagon, because it means they can cut back staff and services and save money, all in the name of the insidiously named BFHI. In addition, hospitals receive free grant money, to the tune of millions of dollars, to push these policies.
I’ve had enough arguments online to know that a decent portion of women don’t agree with my assertions about the BFHI. So before you get your (mesh) panties in a knot, let me address the usual claptrap that gets tossed about.
First, I don’t have any issue with rooming in. Again, if you want to do it, good for you. But again it all comes down to choice. You may not want to use the nursery, but that does not mean I should be prevented from using one.
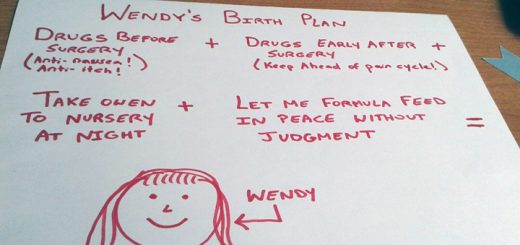
In particular, as a person who has had three c-sections, including one very bad experience, I can attest that the nursery is a necessity, not a luxury. People like to argue that you will be exhausted with the newborn anyways, so you’d better get practicing asap. Why? For what reason, in America at least, are women expected to be superheroes that pop out an eight pound human being and then go about their business like nothing else has happened? In other countries, the mother is allowed days, sometimes a month to recuperate. Moreover, there is a difference between the normal exhaustion that accompanies parents the first few weeks of a newborn life and the exhaustion that occurs after hours of labor and/or a full abdominal surgery. In the case of those women who have had c-sections (which can be upwards of a third of American women), they are taking various narcotics for pain, including morphine and opioids. Guess what the first common side effects listed for these drugs are? That’s right: weakness, dizziness, sleepiness, and sedation. Yet, we are going to hand a newborn to one of these mothers and leave her alone to fight through the drug-induced exhaustion to care for the baby.
Indeed, the health care industry is starting to see the problems with this policy. In an article published in JAMA last month, doctors finally admitted that strict adherence to the BFHI ten-steps may “inadvertently promote potentially hazardous practices”. In particular, the article cautioned that the policy “may inadvertently result in a potentially exhausted and sedated mother being persuaded to feed her infant while she is in bed overnight, when she is not physically able to do so safely.” The risks include a newborn falling out of the bed under these circumstances. (As someone who almost dropped my son on this last go-round due to these practices, I can attest that this does happen).
At this point, let me address a favorite mouthpiece of the naysayers: no, nurses are not there to watch the baby while the mother rests. This is the entire point of well-baby nurseries, which the BFHI is helping to eliminate. Nurses are there to check vitals on the mom and the baby, to ensure that no complications are occurring after the birth with either patient. If nurses are focused solely on the breastfeeding aspect, then they are focused on the wrong thing. Of course, this is becoming the case in more and more BFHI hospitals, as I recently experienced. Because the nurses were hyper-concentrated on whether I was breastfeeding (I wasn’t), and their insistence that I should be, they did not focus on my health, missing complications which almost cost me my life.
As an additional counter argument to one that is often raised: not everyone has family or spouses available to help, either. If you don’t believe me, have a second child. Where is your spouse now? Oh yeah, he’s home with the other kid. Not that he can do much if you are not supplementing or formula feeding.
Which brings me to my final major issue with the BFHI: not all babies benefit from being breastfed entirely or only exclusively after birth. Breastfeeding-only proponents would have you believe that all mothers are able to produce breastmilk at the outset, without any complications. This is patently not true. One only has to glance down the breastfeeding aisle at Babies R Us replete with nipple shields, lactation aids, and stimulating devices to see that this is not the case. Some doctors estimate that the proportion of women who can’t breastfeed is around 15%, as they suffer from conditions such as insufficient glandular tissue. But this doesn’t even take into account women who have suffered from cancer or other conditions that may prevent lactation, let alone women who may eventually start lactating but may not initially, due to premature birth, stressful births, or other conditions.
All of these issues with breastmilk contraindicate a policy that rigidly refuses any supplementation with formula. In fact, some babies who are not getting enough milk in the first few days suffer from jaundice or hypoglycemia, which can in turn affect their neurological growth down the line. In the simplest terms, the BFHI’s policy of refusing formula, even supplementation, to ensure exclusively breastfed newborns, can cause brain damage in these infants. How is that even acceptable?
Of course, I’m not a nurse. So don’t take my word for it. But I did manage to find an anonymous nursing site where OB nurses are expressing concern over these very same policies. At least one nurse has expressed concern that she wondered “how many babies are going hungry while we reassure mothers that their babies are being fed, when in reality they are not.”
That same nurse acknowledged that “Most moms haven’t had adequate sleep since before labor and some are taking narcotics for pain. This is not a safe situation. Most babies are not hurt, but the risk is definitely there. Our fall risk assessments that we complete every four hours even acknowledge that a tired, breastfeeding mother has a higher risk of dropping her baby. Even though adverse outcomes like falls are infrequent, the fact that we are sending new mothers home in states of exhaustion is not acceptable. Most women do not have help at home, and the hospital is the only place they do have some assistance. Instead, they are looked down upon when they ask for it.” Id.
There is an even greater problem with pushing breastfeeding to a point of mental and physical exhaustion: it is going to cause even higher numbers of mothers with post-partum depression and anxiety. This concept is not a stretch: we expect mothers to give birth, stay awake for days afterward to exclusively breastfeed, and to do it alone. This routine would not be healthy for anyone, let alone new mothers.
Because of this, the BFHI has become a hindrance to the health-care of women and newborns. It is the very parable of a good intention that has lost its way. The current practices are neither mother-friendly, nor baby-friendly, despite what the name states. A better policy would be one that supports breastfeeding, while recognizing that it is not the best feeding method for all families. It would be a policy that sees mothers as more than a feeding vessel, and remembers that she is still a patient, too. It would be an initiative which recognizes that the best outcome for a baby flows directly from the physical and mental well-being of its mother, and puts in place steps that value this outcome above any feeding or sleeping methods.
Wendy Marcus
I am mediocre mom!
Latest posts by Wendy Marcus (see all)
- THE ROAD TO HELL IS PAVED WITH LEGOS - April 25, 2017
- Examining Equality in the Practice of Law: The Scales of Justice are Still Not Balanced - April 8, 2017
- Dear America:I think it’s time to consider a divorce - January 26, 2017
















This lady hits the many problems with the BHFI right on the head! When my daughter had her son, she had to have a C-section. She had problems with breastfeeding but they wouldn’t give her any formula. Her son was crying all the time because he was hungry, which caused stress which just complicated attempted breastfeeding. Finally, one of the older nurses said that baby was starving and she didn’t care what they said, she was getting some formula. Meanwhile the baby had lost 14 ounces (almost a whole pound). When they went home, she received a call from the state health people asking whether the baby was being fed. Of course we informed them that the baby was gaining weight since we could feed it formula. The so-called lactation nurse who was supposed to help with the breastfeeding was a total loss. She did not show my daughter how to use the breast pump; when my daughter called for assistance in feeding the baby, the nurse would take up to 45 minutes to an hour before showing up and by that time the baby was so hungry, nothing seemed to help. After they returned home, if she called the nurse for help (which she was told to do), the nurse sometimes didn’t call back until the next day. During the time she was in the hospital, she got very little rest. One of the nurses, again an older one, saw how tired she was and said she was taking the baby to the nursery so my daughter could get some rest.
When my daughter had her baby girl four years later, nothing had changed. However, she was prepared when she went to the hospital. She again had to have a C-section and had problems with breastfeeding. However, this time, she was prepared. She brought her own formula. I stayed with her the first night and was very vigilant to see that she got some rest. Her last night she was in the hospital, her husband stayed with her. He was asleep and she was feeding the baby. Unfortunately, she dozed off and the baby fell on the floor. The hospital took the baby for a “scan” (I assume it was an MRI) to see if the baby was OK. They said she was OK and apparently she wasn’t injured. Then they charged us over $300.00 for the scan, which insurance wouldn’t pay. Because of her C-section, my daughter was also on opiate pain medication and I felt that was why she may have dozed off and the baby fell on the floor, and the fact she had very little sleep during the three days she was in the hospital. One of the nurses told her that having the baby with her 24/7 was good to prepare her when she got home. That’s a crock! In the hospital people are always coming in to check on the baby, take vitals, bring meals, bring menus to order the next day’s meals, take photos, and it is noisy with announcements over the PA and general hospital noises. At least, at home you can nap when the baby naps and it is usually quiet.
I thought this article was wonderful. Unfortunately the medical people who think they know it all won’t do anything to change it. I read recently where a young girl was charged with murder because her baby starved to death. Apparently no one had instructed the girl about breastfeeding problems and she didn’t know the baby wasn’t thriving. Very sad.
While I appreciate and understand all of the problems you see and may have experienced with the BFHI, I feel it is very one sided.
I won’t sit and pick apart everything you have to say about the BFHI because I understand in your case this is how things went. I do want you to understand in return though that not ALL baby friendly hospitals practice this way. If practiced correctly and with the use of critical thinking and a lot of common sense, the BFHI is a beautiful thing. For breastfeeding AND formula feeding moms alike.
I’m an OB nurse with 10 years of experience. I am currently working for a facility on the baby friendly journey. I’ve seen what having a well baby nursery means (for families and faculty alike) and I’ve seen what a strong lack of breastfeeding knowledge and help look like. So I understand part of where you are coming from.
Now for a hospital that is getting it right….Our staff works very hard to insure the health, safety and wellbeing of our families in all aspects, not just breastfeeding. Frankly, I’m offended anyone would think I pay less attention to the health of a mom I’m caring for because I’m too busy trying to get a baby to FEED. I’m actually very much capable of both, as is the rest of our staff.
Notice before that I said FEED? That’s because we want our moms to feed their babies. We want them to be educated on the vast benefits to mother and baby that breastfeeding provides. We understand its not for all moms but we teach them anyway. So they can make an EDUCATED decision. In the end, if they choose, formula is provided to them. Along with education on formula feeding and preparing formula once at home.
As for the well baby nursery issue. Trust me when I say it isn’t a matter of “cost” and staffing to cover it. I’ve worked in facilities that had them and now one that doesn’t. It doesn’t really change our numbers as far as staff goes. There is still an actual nursery. The short of it, if baby is in a nursery, mom doesn’t get a chance to learn to care for her baby. As hospital staff, it would be irresponsible to send a baby home with a new mother when they haven’t assessed her knowledge to care for a newborn infant.
THAT is true baby friendly. I’m sorry for your experience and the woman’s in the comment above. I just can’t sit by and listen to people bash something I feel is so important for our families. When done right it truly is an amazing thing.
I am a night shift OB nurse. I work PP and the NICU. What we are doing to these kids and moms is ridiculous. The fact is that the research does not show breastfeeding to be best. The claims that breastfeeding groups make regarding all of its benefits are unfounded. How much of the “benefits” of breastfeeding are due to psycho-social factors? What about the dehydration and hyperbilirubinemia? There is however research that formula breaks down bilirubin better than breast milk.
Regardless, I am always happy to help a mother breastfeed. I will spend as much time as physically possible if that is what the mother wants. At the same time, I see these poor moms at 3am in tears because their kid wont stop crying. I see the NICU moms breastfeed for 20 min, sit with baby for the top off tube feeding for 30 min, then go back to their room to pump for 20 min. Baby eats every 3 hours. That leaves mom with about 1 hour of sleep between caring for baby, pumping, and taking care of herself. Or what about the parent who is told only breast milk, only breast milk, only breast milk….and then ends up with a hypoglycemic baby? At our hospital parents are as likely to choose IV dextrose over formula supplementation (if BM not available) simply because they’ve been told a baby should never have formula. Yep, you read that right. A parent will choose for us to poke their child with a needle, have it taken to the intermediate nursery and away from family before choosing to try a bottle. And the worst part? No doctor or nurse tells them that’s stupid because we aren’t supposed to. I’m sick of it. But sometimes I’m seen as “against” breastfeeding by our lactation staff because of it. How absurd.
If having informed patients is so important (it IS!) then parents should be informed of ALL of their options. So many parents seem to feel it’s all or nothing. You breastfeed or you bottle feed, no in-between. That’s simply not the case but they don’t know that and we as OB nurses are not allowed to tell them because it’s not “baby friendly”.
I brought a study to my supervisor that showed healthy term infants who received small amounts of formula in the first few days of life had better breastfeeding rates at 6 months. Unfortunately, my hospital is working on acquiring BFHI status. It ended up in the recycling bin without anyone besides that supervisor reading it.
I would love to put a poster on our unit with a survey of nurses and their feeding choices for their own children. I would bet money that at least half would be giving their child some amount of formula at some point in the first few weeks. Personally, I would not only not hesitate but I would PLAN to use formula until full milk production! I know many of my coworkers would agree or at least not be opposed to supplementing/pacifier should the desire to do so arise during their hospital stay.
Please know, there are many OB nurses who agree with frustrated parents. We don’t like it any more than you do but going up against hospital administrators and fanatical breastfeeding supporters is extremely difficult when your job may be at stake if you push too hard. Keep your voices heard. Administrators will listen to the people who pay the hospital bill! Thank you for your awesome original post!
BFHI does not force mothers to sign waivers if they choose to breastfeed. This is simply not a requirement. BFHI wants you to educate the mothers on the benefits of breastfeeding and then they can make their choice. If the mother chooses to feed formula, that is her right to do so. You simply have to document that the mom was educated and chose to formula feed. In our facility, mom’s choice is respected as we move through our baby friendly journey. The statements made in this article are not 100% true according to baby friendly guidelines. People need to learn the truth from BFHI not from random articles published on the Web.
While I respect that your experience may be different, the fact remains that I have experienced firsthand some of these issues with the BFHI. I have also spoken or written with women who also were forced to sign waivers, had formula withheld despite request, and/or treated negatively because they chose to formula feed. The fact that these scenarios exist in different health care facilities trying to follow BFHI guidelines demonstrates, at a minimum, a serious disconnect in how the initiative should be implemented. I take issue with your phrase that “people need to learn the truth from BFHI” because it somehow implies that my experience, and the experience of these other women, either did not happen, were random outliers, or should be ignored for the good of the BFHI. The point of my article is that the BFHI is the example of a good intention that has, at least in some facilities, overtaken the mental and physical well-being of the mother, which should be paramount.
Yes they do require mothers to sign waivers. If they don’t they are not adhering to the real Baby Friendly guidelines.
Baby Friendly has become a policy based on coercion and making mothers feel guilty and not allowing them to make an educated decision about what is best for themselves and their babies.
As a physician I have seen delayed diagnosis of serious medical issues in newborns ranging from congenital heart disease to hypoglycemia because the medical concerns of the mother and infant become secondary to the goal pf forcing everyone to breastfeed.
Any nurse who negates the fact that the biologically normal food for a human is not the best food should have her license pulled. I’m talking to you Lynne. The fact that you’re a PP nurse is FRIGHTENING. Take just one lactation course. It should be required of you in order to be a PP nurse. It pains me to think of the number of breastfeeding relationships derailed by your ignorance.
Any nurse who pushes breastfeeding above every other factor including the health and well-being of the mother should have HER license pulled. Just saying.
I’m not sure you understand the public health risks that come from feeding humans corn syrup & vegetable oil and acting like it’s food.
I’m not sure you understood the entire point of this article.
I don’t even understand how I ended up right here, but I thought this put up used to be good.
I do not understand who you are but certainly you are going
to a well-known blogger if you aren’t already.
Cheers!
I couldn’t agree more with everything written in this article. We are planning to have our third child soon. I live in a small city with only one hospital and I am really upset that they are part of the BFHI, especially because we don’t have family in the area and, with two other kids, my husband will not be able to stay overnight. They have done away with the well-baby nursery, and I have heard terrible stories from other mothers who had to practically beg the nurses to take the baby for an hour so they could sleep. It’s not the nurses’ fault–all they can do is take the baby on their rounds since there is no room for them. They have a “volunteer program,” which means that there are about four hours a week where you have the option of handing your baby to a complete stranger with no medical training whatsoever who will take your baby to the lounge. I would laugh if I didn’t feel like crying at the prospect of getting no relief after going through labor, right before going home to a house with three kids.
And don’t even get me started on the insane pressure to breastfeed. If you ever want to read something really creepy, read the guidelines and criteria for the BFHI–it is so intrusive and Orwellian (I’ve posted some excerpts below). Unfortunately, I don’t have a choice. I even googled for other hospitals nearby, but the closest one is almost two hours away. Driving two hours in labor with my third baby? Not going to happen. So BFHI it is—whether I like it or not.
Here are some excerpts from the BFHI guidelines:
“All areas of the facility that potentially interact with childbearing women and infants will have language in their policies about the promotion, protection, and support of breastfeeding. Policies of all departments will not countermand the facility’s breastfeeding policy.” – I guess that means you can’t hang up a “Fed is Best” poster 😉 or really anything that puts women’s mental health above insane lactation goals or provides emotional support to women who can’t or don’t breastfeed??
It goes on with a long list of “80% of women” this and that, including such inane details as, “Observations of vaginal births … show that (regardless of the mother’s feeding intentions) at least 80% of infants are placed skin-to-skin with their mothers within 5 minutes after birth and are held continuously skin-to-skin until completion of the first feeding, or for at least one hour if not breastfeeding.” – Don’t get me wrong, I loved holding my babies after they were born, and I do think it’s important to make it easy for mothers and fathers to stay together and have some special, quiet time after birth. But why prescribe one way as the “best”? It’s also ok to hold the baby in a blanket (duh!), to hand the baby to your partner or to simply rest for a little while. (I did all of these things and went on to breastfeed both of my children.) There is no right or wrong. How about simply stating that mothers should have options and the space to follow their own heart? (But of course, we’ve seen that the BFHI is not big on giving women actual, true choices.) And why is this intimate moment figuring in some hospital statistic at all, with percentage goals attached to it? I mean, seriously??
And, of course: “Each facility should track its rate of formula supplementation of breastfed infants. […] In addition, a year-by-year reduction in non-medically indicated supplementation is expected in Baby-Friendly designated facilities.” – So this is what my hospital is supposed to be focusing on now? How about making sure me and my baby are healthy and supported? Oh, and where or when is that “expected” trajectory supposed to end – at a 100% breastfeeding rate?? Even in Saudi Arabia, where women are forced to breastfeed by law, the actual breastfeeding rates are way below that. Do I need to say more?
And, the gem: “When a mother specifically states that she has no plans to breastfeed or requests that her breastfeeding infant be given a breast milk substitute, the health care staff should first explore the reasons for this request, address the concerns raised, and educate her about the possible consequences to the health of her infant and the success of breastfeeding. If the mother still requests a breast milk substitute, her request should be granted and the process and the informed decision should be documented.” – I guess this is the fun part where exhausted new mothers can be exhorted to explain and defend their personal feeding decisions to every staff member they meet. Oh, and let’s not forget about the shame-inducing (and often scientifically inaccurate) forms where formula-feeding mothers have to sign that they really belong in mothering hell… ah, no, that they willingly choose to endanger their baby through the dangerous practice of formula feeding, of course. It’s “heaven for bullies” week at the BFHI! Tsk, tsk, women just can’t be left to make their own decisions, can they? *snark*
Oh, and just in case anyone has not gotten with the program yet: “Of breastfeeding mothers whose infants have been given food or drink other than breast milk, at least 80% of those who have no acceptable medical reason will report that the health care staff explored the reasons for and the possible negative consequences of the mother’s decisions.” — Those naughty, naughty mothers who choose to supplement without having an “acceptable medical reason”…
And it just goes on and on… It’s as if maternal and fetal health hinged on breastfeeding and nothing else. This is what happens when you have a philosophy where women’s choices are ignored (“oh, she must not have educated herself enough”), where women’s wishes don’t matter, and where possible downsides of breastfeeding, as well as actual dangers to mothers (exhaustion, mental health, PPD) and babies (hunger or worse), are at best an afterthought.